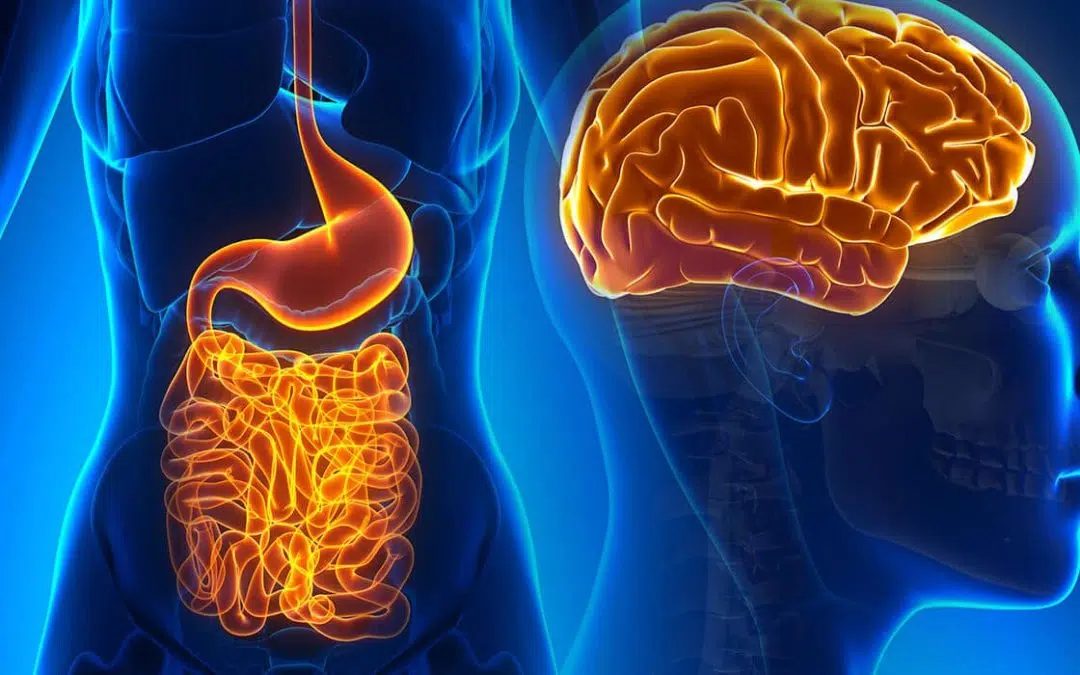
What is the gut-brain axis, exactly?
Don’t worry, no graphing paper or calculator is needed for this one. However, the answer is possibly no less complex or mind-blowing than high-level mathematical theory, either.
In the scientific community, some have taken to calling the gut-brain axis “the second brain” colloquially or more formally – the “Enteric Nervous System” (ENS). This vast communication network refers to over 100 million nerve cells that line our gastrointestinal tract which actually begin in the sinuses, not the gut. This “second brain” is a communication channel for your whole body, and is deeply entrenched in, and connected to, important facets of your wellbeing. When it’s out of sync, communication can break down and trigger health issues. Like so many rom-coms have shown us, miscommunication leads to trouble.
Take the vagus nerve for example, one of the biggest nerves connecting your brain and your gut. Recent studies have shown that psychological stress can harm the vagus nerve and its ability to function as a two-way communication channel, which can lead to the development of gastrointestinal disorders, like IBS.
What does the gut-brain axis do? Why do we have one?
The more research emerges, the more we understand just how deep the connection between our gut and our brain (hence, the gut-brain axis) truly is. While studies are ongoing and our comprehension of the gut-brain axis is fairly new, all signs point to the gut-brain axis being extremely important to our health and wellbeing.
One exciting development is that we now know that a large percentage of the body’s neurotransmitters like serotonin and dopamine are produced in the gut, not the brain. Neurotransmitters are the chemicals by which your gut and brain communicate. Neurotransmitters are responsible for regulating emotions, including the “fight or flight” response and, recent studies show, can also affect blood flow, bowel movements, nutrient absorption, the immune system, and the body’s microbiome.
When these neurotransmitters are thrown off, the disruption may result in inflammatory gut conditions and diseases but can also possibly lead to neurodegenerative problems as well. That’s because this deep connection between the gut and the brain have profound effects on one another, and why something like poor gut health can be partially attributed to (if not fully responsible for) the onset and progression of many mental disorders, including depression, schizophrenia, autism, epilepsy, and even migraines. This may also be why studies have shown that those with good gut health are shown to be more resilient to the negative impacts of stress and external pressures.
The answers for why mental health is connected to gut health via the gut-brain axis can be found in our microbiome – the bustling, thriving, unique ecosystem where countless viruses, fungi, microbes, and bacteria live together and help keep our bodies in balance. The gut microbiota in our bodies play a huge role in our health throughout our entire lives, starting from when we are born (literally!). Multiple studies have shown changes to the gut microbiota in early life–via antibiotic exposure, lack of breastfeeding, birth by C-section, infection, stress, and other environmental influences–can result in long-term effects on physiology and behaviour and affect the gut-brain axis.
What can disrupt the gut-brain axis?
The gut microbiome develops at the same time as the central nervous system, but birth and early life aren’t the only times the gut microbiota (and by extension, the gut-brain axis) can be affected and changed. Everything from our environment to what we take antibiotics (and more) can have an effect on our gut microbiome.
So, to put it simply: if it’s bad for the gut, it’s bad for the gut-brain axis.
A poor diet, stress, antibiotics, gluten, genetics, glyphosate and other environmental toxin exposure can all negatively affect the health of the gut and, by proxy, affect the ability of the gut-brain axis to function properly–which means a whole host of things are at risk of not functioning properly as well.
Emerging evidence suggests that an off-kilter gut-brain axis may even change the metabolism, affecting eating habits, satiety, and weight management. An interesting study conducted in 2020 showed that a disrupted gut-brain axis can create a strong preference for the taste of sugar, even. (As if resisting excess sugar wasn’t already difficult enough.)
But there’s far more, far-reaching consequences that can occur when the gut-brain axis pathways are thrown off. A big one to consider is that the physical barrier between the central nervous system and the cardiovascular system (the blood-brain barrier) can become more porous with a disrupted gut-brain axis. When this barrier leaks, it can lead to neuroinflammation of the brain and manifest as a variety of serious health issues like Alzheimer’s and Parkinson’s disease.
What can you do to improve (and protect!) your gut-brain axis?
If you’re interested in improving your gut-brain axis, one of the most important things you can do is improve your gut health. And one of the easiest ways to do that? Start with your diet.
Dr. Megan Rossi, founder of The Gut Health Doctor says: “For a simple idea of how to improve your gut health naturally, aim for at least 30 different plant-based foods a week, full of fibre and beneficial plant chemicals. The more diversity, the better.”
While you’re aiming to get your nutritious meals in, there are some foods that are especially adept at helping improve gut health to keep top of mind:
Omega-3 fatty acids
These fatty acids are essential fats that the body cannot produce, so we must get them via food. (Oily fish like salmon are great sources for omega 3’s.) These fats are unique in that they can change the structure and function of cell membranes, and have a large swath of benefits, from improved cardiovascular and metabolism function to better gut health. They have even been shown to reduce the risk of brain disorders.
Fermented foods
Fermented foods–including yogurt, sauerkraut, and cheese–all contain healthy microbes including lactic acid bacteria which are good for gut health.
High-fibre foods
There are many reasons high-fibre foods are good for you. A big one is that high-fibre foods like nuts, whole grains, seeds, fruits, and vegetables contain prebiotic fibres that your gut bacteria love. (Also, prebiotics can reduce stress hormones!)
Polyphenol-rich foods
These naturally occurring organic compounds from plants have a multitude of beneficial influences on one’s health, including increasing healthy gut bacteria and improving cognition – thanks to their anti-inflammatory and antioxidant properties. Cocoa, green tea, and olive oil are all polyphenol-rich foods.
Tryptophan-rich foods
Most of us think of turkey when we think of tryptophan, but eggs and cheese are also high in this helpful amino acid. How helpful? It converts into serotonin, a crucial neurotransmitter.
Contact us to make a booking or to enquire.